In an effort to reduce hockey injuries, research studies have been undertaken in order to better understand the risks and to implement preventative measures. Rule changes, enforcement of existing rules and protective equipment standards are attempts to improve the safety of the game. Attention has been also been directed toward education of coaches, players, parents, and officials. Potentially dangerous actions such as checking from behind and the use of the helmet or the stick as a weapon must be eliminated from the game.
Prevention is the Key
The intrinsic hazards of playing hockey cannot be completely eliminated; but the risk of injury can be substantially reduced. Fortunately, the overwhelming majority of hockey injuries are mild. Most injuries involve the soft tissues: bruises (contusions), muscle pulls (strains), ligament tears (sprains), and cuts (lacerations). Serious injuries are possible and players should avoid dangerous tactics:
Never
- Deliver a hit to the head
- Check from behind
- Drop your head near the boards
- Leave your feet to give a check
- Use your stick as a weapon
A preseason screening examination by an experienced athletic trainer or physician may identify existing injuries and uncover deficiencies. Sports specific conditioning avoids physiologic overload, which can result in overuse injury. Effective stretching decreases the risk of soft tissue trauma such as a muscle strain. Proper fitting, quality equipment is essential for all players. Although players are often resistant to equipment changes, damaged, worn-out or undersized equipment may be ineffective. Post-injury evaluation ensures appropriate treatment and guidance on safe return to play. Hockey players should have an appreciation for the types, locations, and mechanisms of the more common injuries in order to implement preventative measures.
Head and Face
Mandatory use of standardized helmets has apparently reduced the incidence of severe head injuries with brain damage. Concussions do occur and players should always report symptoms such as prolonged headache, confusion, visual disturbance, and loss of memory or concentration. Concussions encompass a graded set of clinical syndromes that may or may not involve loss of consciousness. A direct blow to the head, face, neck or elsewhere on the body causes concussions by transmitting an impulsive force to the head. The resultant brain injury is due to a rapid onset, short-lived impairment of neurological function that resolves spontaneously. The acute symptoms reflect a functional disturbance rather than a structural injury. A recurrent blow to the head can be serious, since repeated concussions cause cumulative damage and the severity increases with each incident. After an initial concussion, the chance of a 2nd concussion is four times greater.
Players, coaches and parents should be aware of the typical symptoms and sign:
Symptoms- Unaware of Situation
- Confusion
- Amnesia
- Loss of consciousness
- Headache Dizziness
- Nausea
- Loss of balance
- Flashing Lights
- Ear Ringing
- Double Vision
- Sleepiness
- Feeling Dazed
- Loss of Consciousness
- Altered Mental Status
- Poor Coordination
- Slow to Answer
- Poor Concentration
- Nausea or Vomiting
- Vacant Stare
- Slurred Speech
- Personality Changes
- Inappropriate Emotions
- Abnormal Behavior
Whenever evaluating a player with a suspected concussion, always rule out an associated neck injury. The examiner should put a hand on either side of the head to stabilize the neck until the exam is complete. Do not move the athlete, remove the helmet, rush the evaluation or worry about delaying the game. In the player is unconscious, use the log roll method to turn the player supine, leave the helmet and chinstrap attached, and begin cardiopulmonary resuscitation (CPR) as necessary. After a neck injury has been ruled out, help the player to the bench or locker room. Perform a “sideline” evaluation, and then repeat after 15 minutes at rest and after exertion. No grading system or return to play guidelines to date has been validated. Common sense and caution guide judgment. A symptomatic player should never return to play or be left alone. The player should be monitored regularly, medically evaluated after the injury and again before returning to play.
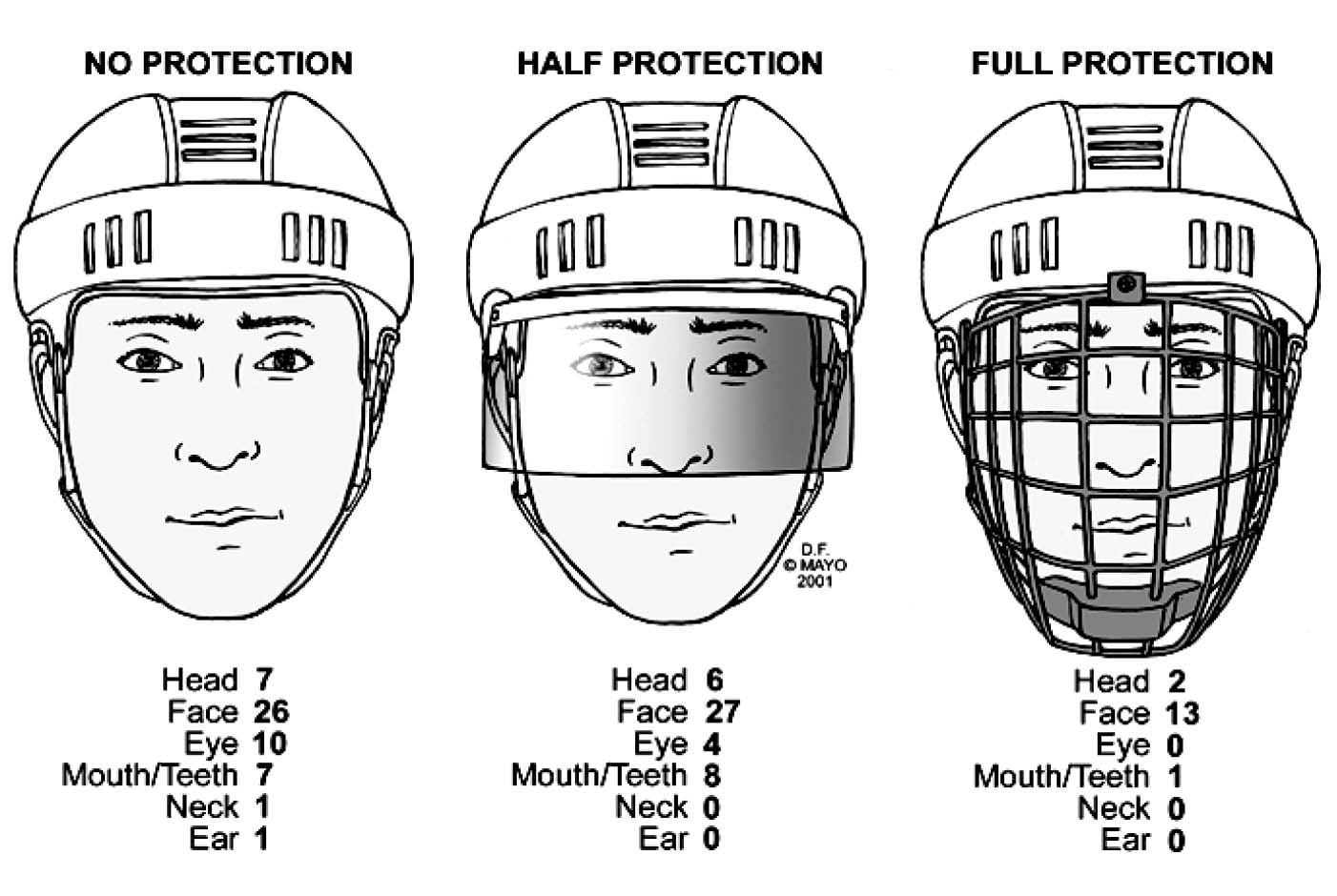
Facemasks have dramatically reduced the risk of eye injuries, including blindness, and lacerations (cuts). No permanent eye injury has been reported to a player wearing a certified mask. Full facial protection for all participants may reduce the risk of facial lacerations, dental fractures (broken teeth), and potentially serious eye injuries.
Neck
Serious neck injuries (cervical spine fractures) are usually the result of a direct blow to the top of the head (axial load) with the cervical spine slightly flexed (chin down position). This mechanism occurs in hockey when a player slides on the ice without control or is pushed or checked from behind and hits the boards. The risk of spinal cord injury, including quadriplegia or complete paralysis, may be increasing and appears to be higher in hockey than football. Helmets and facemasks have been implicated in this apparent increased incidence of neck injuries because players feel invincible and officials are more lenient in calling penalties. No scientific research to date supports these contentions. However, a false sense of security may lead to violent attitudes and tactics. Prevention of catastrophic injuries involves the cooperation of players, coaches, and officials. Dangerous violent acts must not be disguised as aggressive physical play. Players should learn to protect themselves by making initial board contact with another part of their body other than their head. When sliding on the ice or being checked near the boards, try to make board contact with the shoulder blade or buttock areas. If head contact does occur, players should avoid the position of vulnerability by always keeping their “heads up” (in other words: “don’t duck”). Coaches should teach body contact and control skills so that players can effectively and safely give and take checks. Athletes and coaches must always practice the objectives of sportsmanship, including respect for their opponents. Conditioning programs should include strengthening of the neck muscles. Existing rules, like checking from behind, charging, and boarding, must be strictly enforced. Non-officials (players, coaches, and fans) must support the on-ice officials who are trained to differentiate illegal from legal contact in order to eliminate dangerous actions. A larger ice surface (“Olympic-size” rink) may decrease player-board contact, which may decrease the risk of injury, especially to the head and neck.
Shoulder
One of the most common injuries in hockey is a shoulder separation (acromioclavicular joint or AC sprain). The ligaments connecting the shoulder blade (acromion) to the end of the collarbone (clavicle) are stretched or torn. This injury occurs when the point of the shoulder (acromion) hits the boards or another player. Recovery from a mild sprain may take only a week, but a severe sprain can keep a player out of action for a couple of months. In younger players, the same mechanism can cause a clavicle fracture (broken collarbone). Protection is best with proper size shoulder pads that provide a cushion to dissipate the force. Players can also try to avoid dropping their shoulder when a collision with the boards is inevitable. A shoulder dislocation (glenohumeral dislocation) refers to the ball of the shoulder joint popping out of the socket. This injury occurs when the elevated arm is forced backward (cocking position) or from a direct blow to the back of the shoulder. A period of immobilization, strengthening exercises and bracing may help prevent a recurrent dislocation, but surgery is often required to tighten the torn ligaments and joint capsule.
Elbow
The point or the elbow (olecrannon) is a frequent area of contact, which can result in the development of bursitis. This condition is not usually severe, but can cause pain, swelling and fluid formation (effusion) in the bursal sac. Thick and scarred bursal tissue (which feels like bone chips, but isn’t) can be a source of recurrent inflammation. Elbow pads that fit well (don’t slip down) and have an opening for the olecrannon, soft padding, and a hard plastic outer shell work best.
Wrist and Hand
A fall on the outstretched arm or bracing against the boards with the hand can cause a fracture of the scaphoid bone or the end of the radius (in younger players). A dorsiflexion (backward) force transmitted to the wrist can also sprain the ligaments between the wrist and hand (carpometacarpal sprain). The thumb is also at risk for injury because of the grip required to hold the stick. An abduction force (away from the hand) can tear the ulnar collateral ligament at the base of the thumb (ulnar collateral ligament sprain). A partial tear is treated with a splint and taping; but a complete tear may require surgical repair. Hockey gloves provide some protection for the hand from direct blows (slash) that can cause finger fractures. Gloves that are worn out may not provide the necessary support for the thumb or protection for the hand.
Back
Hockey players are at risk for low back injuries due to the flexed (forward) posture of skating and the frequent hyperextension (backward) stress. A pulled muscle (lumbar paraspinal muscle strain) is the most common result, but a stress fracture of the posterior spinal elements (spondylolysis) must be considered if the pain doesn’t respond to the usual treatment measures. Stretching of the paraspinal muscles and strengthening of the back and abdominal (stomach) muscles will help avoid these injuries.
Hip
The mechanics of the skating stride makes the hip and groin muscles susceptible to injury. Some of the most common soft tissue injuries in hockey players include a groin pull (adductor muscle strain) and a hip flexor pull (rectus femoris or iliopsoas muscle strain). A severe strain can be a nagging injury that limits performance throughout the season. Offseason strengthening and dedicated stretching each day (before and after practice) are important to prevent these injuries. A direct blow to the outside of the hip can cause a bruise (contusion) of the iliac crest (hip pointer) or trochanter (trochanteric bursitis). Hockey pants with reinforced padding over these areas may help protect these vulnerable areas.
Thigh
A thigh bruise (quadriceps contusion) can result when the opponent’s knee strikes the thigh below the margin of the hockey pants. A deep bruise with bleeding into the muscle can be a disabling injury. Immediate treatment with immobilization in full knee flexion, crutches, and ice can reduce the bleeding, swelling, and pain. Gentle active range of motion exercises within the limits of pain and control of inflammation is essential to prevent increased bleeding and the formation of calcification within the muscle (myositis ossificans).
Knee
The medial (inside) knee structures are most susceptible to injury (medial collateral ligament sprain) because of leg position (pushing off the inside edge of blade) and frequent contact to the lateral (outside) of the knee. An isolated medial collateral ligament sprain is treated without surgery, but a complete tear requires approximately 8 weeks to heal. Anterior cruciate ligament (ACL) disruption and meniscus tears (torn cartilage) can also occur but are less common in hockey than other sports such as football, soccer, and basketball. A direct blow to the front of the knee can cause a bruise (patellar contusion), inflammation of the bursa (pre-patellar bursitis) or rarely a patellar fracture. Re-enforced shin guards with padding over the front of the knee may provide an important cushion.
Ankle
The sharp skate blade can cut the lower leg above the top of the skate (boot top laceration). A deep laceration can injure the tendons that control movement of the ankle and foot. Players should tuck the tongue of the skate under the shin pad in order to protect this area from the blade. Fortunately, the skate boot supports the ankle, which makes fractures and sprains less common in hockey than other sports. A direct blow from the puck can rarely cause a fracture of the ankle (malleolus fracture) or foot (metatarsal fracture).
In summary, enforcement of existing rules, which will minimize dangerous behaviors, can reduce injury risk in the great sport of ice hockey. Athletes who focus on stretching and strength training are less likely to sustain soft tissue injuries. Players should always demonstrate sportsmanship and mutual respect for their opponents and the officials. Development of body contact and body control skills is essential in addition to stick handling and shooting proficiency. Full facial protection and a custom-fit mouthpiece protect the face and teeth. Improved equipment design may better safeguard hockey players. Rink modifications, such as an increased ice surface size as well as force-dissipating boards and glass will reduce collisions.
Ice Hockey players should always strive to:- Have Fun
- Play Hard
- Play Smart
- Play Fair